The National Institute on Minority Health and Health Disparities (NIMHD) hosted a two-day online workshop, “The Role of Work in Health Disparities in the United States,” to understand and address the role of work as a social determinant that contributes to health disparities. This multidisciplinary workshop convened experts from the research fields of health disparities, population sciences, labor economics, occupational health, epidemiology, and organizational sociology and psychology to consider work as a social determinant and to identify priority research areas, potential mechanisms, and interventions to address the role of work in health disparities.

Workshop co-chair Rada Dagher, Ph.D., M.P.H., Scientific Program Director in Clinical and Health Services Research at NIMHD, and co-chair Nancy Jones, Ph.D., Scientific Program Director in Community Health and Population Sciences at NIMHD took turns leading the meeting over the two days and moderating the sessions. NIMHD Scientific Program Directors Rina Das, Ph.D., and CDR Nadra Tyus, Dr.PH, M.P.H., helped moderate two of the workshop sessions. Sessions were followed by question and answer rounds and lively discussion among the presenters and participants.
The first day of the workshop, introduced by Dagher, provided an overview of the current knowledge and conceptual grounding of research on work and health disparities, addressing:
- Theoretical foundations.
- Concepts, measures, indicators, and analytical approaches.
- The challenges of operationalizing the concept of work.
Day two, introduced by Jones, addressed:
- Key mechanisms such as occupational segregation, worksite segregation, life course and intergenerational transmission.
- Systemic-level influences and pathways.
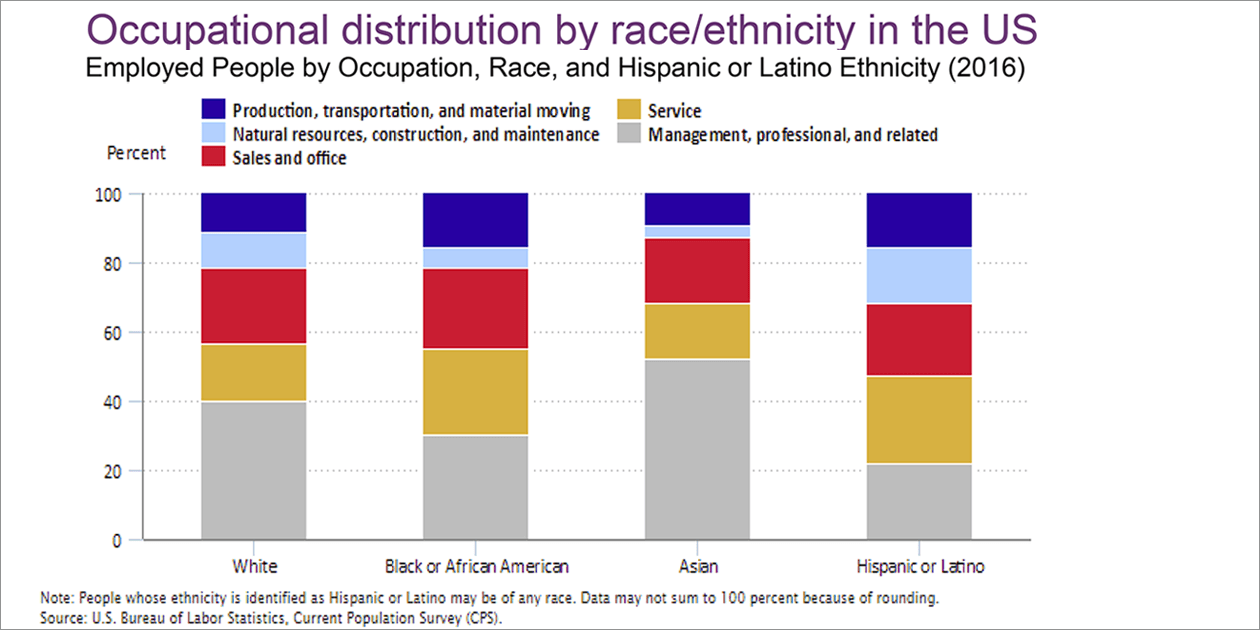
For U.S. adults, the experience of work is strongly influenced by their social identities, such as race/ethnicity, immigrant status, socioeconomic status, gender, sexual minority status, and rural/urban residence. All these factors are associated with health disparities. However, most occupational disparities research to date has focused on hazardous exposures in the workplace. Meanwhile, health disparities research has seldom studied the role of work in explaining health disparities.
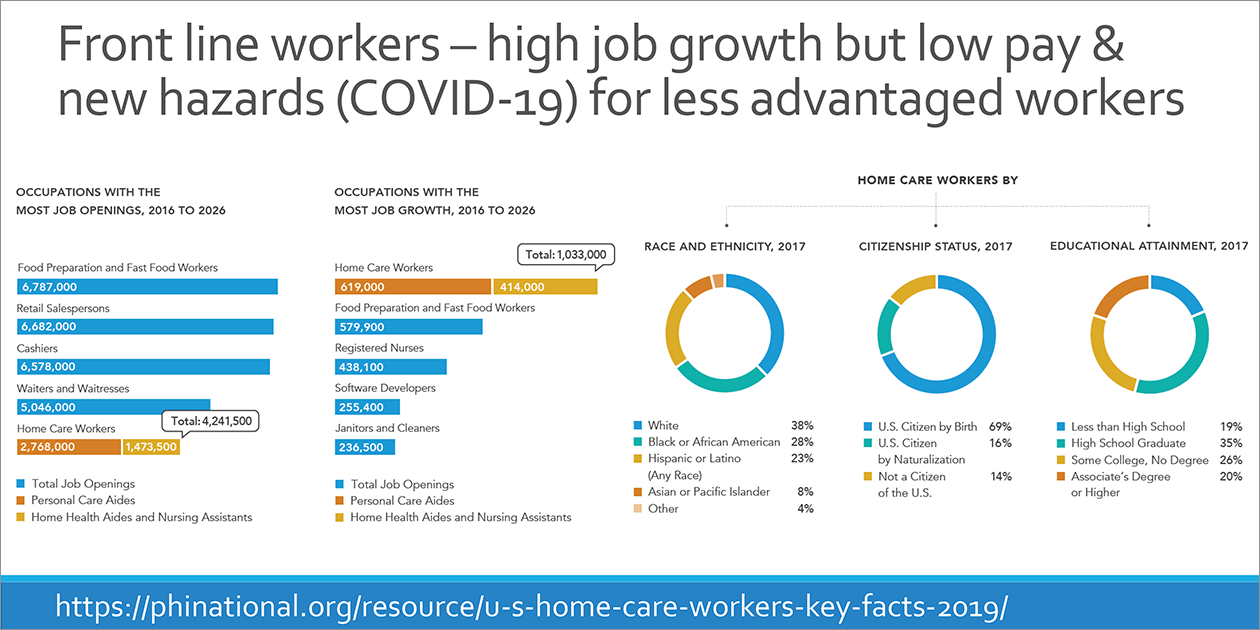
In her introductory overview of the workshop, Dagher stated that studying the contribution of work to health disparities can help tackle a number of disparities underlying current health crises in the United States, such as COVID-19, maternal mortality, and opioid use disorders. For example:
- Do greater membership in essential careers and the related lack of opportunity to telework contribute to higher rates of COVID-19-related severe illness and death among racial/ethnic minorities?
- Do adverse working conditions and unequal leave benefits lead to increased maternal mortality among African American women?
- Do occupational segregation and less employment stability among minorities contribute to greater rates of opioid use disorders?
NIMHD Director Eliseo J. Pérez-Stable, M.D. gave welcoming remarks at the start of day one. He noted that work is a social determinant that may explain a considerable amount of health disparities for race/ethnic minority and low socioeconomic status populations. It is hard to tease out and assess the impact of physical and environmental factors on health outcomes, as they may be confounded by social stressors, behavior, or differences in health care. Conversely, the impact of psychosocial factors may be confounded by physical and chemical exposures in the workplace and in daily life.
“We acknowledge that work and occupation are primary social determinants of health. One of the questions I want to see discussed in this workshop is, how does this differ from what we already get from socioeconomic status, race, ethnicity, and place....I want the group to think clearly on these issues and not take anything for granted.” said Pérez-Stable.
Sarah Burgard, Ph.D., from the University of Michigan, gave the keynote address, “The State of the Science for Research on Work and Health Disparities.” Burgard explained that work had not been studied as a social determinant of health as much as, for instance, education because it is challenging to measure the effects of work on health across the lifespan; most influences appear over time and can be connected to the complex paths of many different aspects of work. Some issues that deserve more attention go beyond individual experiences, to work’s collective impact on families, generations, and communities; as well as the role of an aging workforce and rising retirement age. Macroeconomic issues include labor globalization, economic downturns, weather and health emergencies, and their effects on work opportunities, hazardous exposures, and protections.
Prominent epidemiological sociologist Bruce Link, Ph.D., University of California, Riverside, presented “The Importance of Work in Fundamental Cause Theory,” in which he discussed how work structures major health-relevant aspects of our lives as a source of flexible resources such as money, knowledge, prestige, power, and beneficial social connections, as well as a source of exposures and an important place where racism/discrimination occurs. Fundamental cause theory initially sought to explain how low socioeconomic status leads to persistent health inequalities over time because these communities continue to lack resources such as money, knowledge, prestige, power, and beneficial social connections to protect and improve their health, even when modern public health advances should have helped everyone—not just well-off people—avoid certain diseases of poverty.
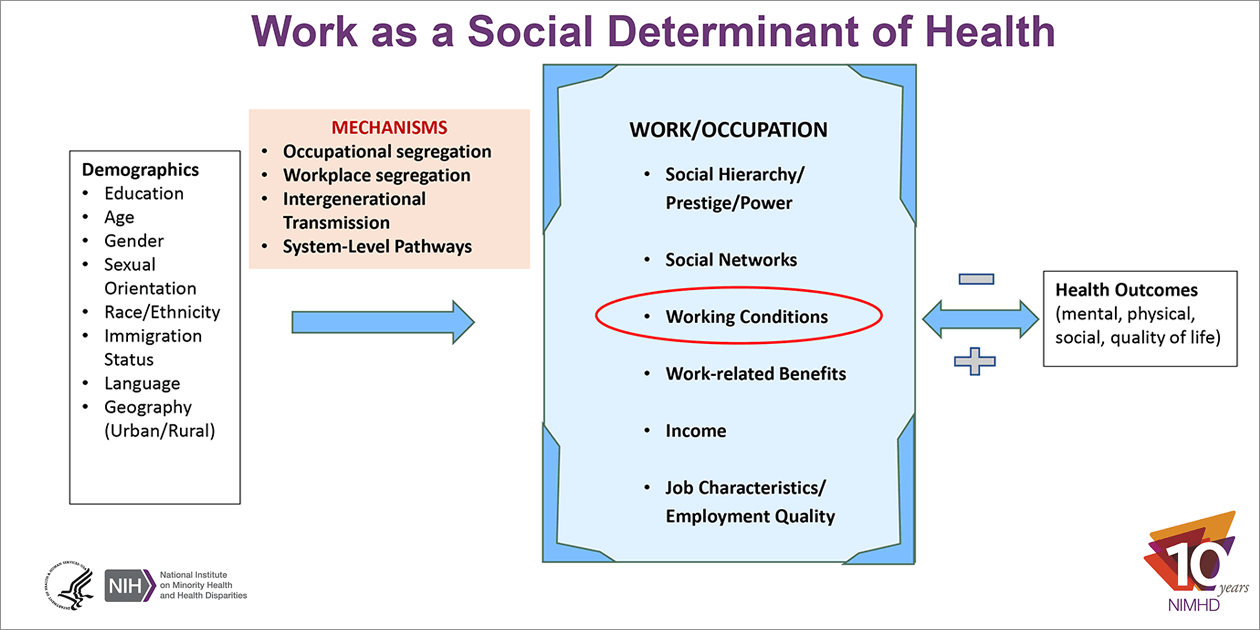
Following Link’s presentation, Dagher presented a related theoretical framework in her presentation “Work as a Social Determinant of Health: Theoretical and Practical Considerations,” where she discussed how work is a multifaceted concept, many aspects of which account for it as a social determinant of health. It is a source of income, health insurance, prestige and power, social support networks, and not only working conditions but also work-related benefits (including leave, job flexibility, and pension). However, “racism and discrimination may underlie the unequal distribution of all the aforementioned resources and conditions.”
Prominent life course sociologist, Phyllis Moen, Ph.D., University of Minnesota, presented “Disparities and Dynamics: A Life Course Approach to Work and Health in Later Adulthood,” in which she encouraged researchers to think of the relationship of work and health as pathways and processes that “unfold over time” and as “dynamic synergies each affecting the other.” Work and health processes not only intersect with one another but also with various family and personal issues. For example, a policy change or the occurrence of the COVID-19 pandemic will have different effects on individuals’ work and health depending on when they occur in their life course and depending on their personal and family situations. Thus, it is important to recognize that the paths of work and health are shaped by the situational demands and challenges individuals experience at a particular point in time. In addition, due to structural inequalities and systems of privilege, individuals’ social identities (e.g., race/ethnicity, gender, immigrant status) influence their locations or positions in society which have profound impact on their work experiences. Moen concluded by asking, “What are the inequality generating mechanisms that constrain choices around work and health and climates of racism, classism, sexism and ageism and how can we develop policies and practices that ameliorate those effects?”
Key ideas for furthering research on work as a social determinant of health include conceptualizing work as a:
- Social class marker.
- Source of “exposures and risk factors.”
- Source of beneficial social and economic resources such as income and wealth, neighborhood conditions, health care access, education, and social networks.
Research priorities include:
- Exploring the degree to which occupational segregation (the unequal distribution across occupations according to social identities) and worksite segregation (the unequal distribution of resources and exposures within the workplace) contribute to health disparities for gender, race/ethnic minority populations, sexual and gender minorities, underserved rural populations, socioeconomically disadvantaged populations, and immigrants, and the mechanisms through which they explain health disparities (e.g., hazardous conditions, unequal distribution of benefits).
- Examining the trajectories of individuals in minority- and low socioeconomic status-concentrated occupations and how they influence the achievement of life goals and optimal health, as well as evaluating how upstream policies, regulations, and system-level trends influence the relationship between work and health disparities.
By the end of the workshop, organizers, speakers, and discussants agreed that the workshop was a great success, sparking groundbreaking discussion of new approaches and interdisciplinary synergies to the underexplored effects of work on health disparities. Jones said, “This is the beginning of the conversation, and we want as much input as possible about what would be areas to explore, prioritize, so that we can understand the role of work as a social determinant that contributes to health disparities.”
Access the workshop videocast and presentations at The Role of Work in Health Disparities in the United States Workshop.
Page updated July 2, 2021
Workshop videocast and presentations
NIH Record: NIMHD Workshop Explores Effects of Work on Health Disparities
Workshop Videocast
Workshop Contacts:
Dr. Rada Dagher
Rada.Dagher@nih.gov
Dr. Nancy Jones
Nancy.Jones@nih.gov